How to Boost Hospital Revenue by Optimizing Hospitalist Case Mix Index Documentation
As hospital margins shrink, hospital leaders seek strategies to enhance revenue. Accurately capturing Case Mix Index (CMI) is a prime way to do just that. The key? Physician documentation. At each of our partner hospitalist programs, we see consistent improvement in CMI by focusing on physician documentation education and mentoring. In this post, we explain the importance of CMI documentation optimization and how to leverage it to help hospitals increase collections.
What is CMI?
CMI is the average sum of the relative weights (RW) of all patients treated in a facility in a specified time. It measures resource consumption and cost of providing care at a facility. When a hospital has a higher CMI, they treat more complex, sicker patients and receive higher reimbursement rates.
Why is CMI important?
Facilities with higher CMI receive more insurance reimbursement. Thus, the higher the CMI, the lower the adjusted cost per patient per day for the hospital.
How to Improve CMI through Documentation
Physician documentation has a direct impact on CMI. When physicians accurately portray the acuity of their patients, it equates to CMI and more reimbursement for the hospital. The most effective way to improve CMI is thorough documentation training and consistent follow-through as it relates to ongoing documentation review and education.
Documentation Training During Onboarding
We suggest robust onboarding documentation and coding training led by a certified coder who is up-to-date on the latest CMS measures and common opportunity areas for documentation improvement. At our partner facilities, emergency medicine physician and certified coder Larry Halem oversees documentation training. Our inpatient training program includes 3 lectures that are 90 minutes total. These are required for all new hires.
The inpatient documentation training focuses on educating providers on the commonly down-coded areas of charts, including:
- Evaluation and Management levels (E+M) and the RVUs associated with each
- Documenting past medical, family, and social history
- Physical exam levels
- Medical decision-making impact on documentation
- Discharge documentation
When it comes to documentation, it is often very fine differences in medical decision making, coding, and documentation that have a significant impact on reimbursement.
“We want physicians to understand what goes into CMI so that they can appropriately document and help the hospital and group be effective inpatient collections,” said Halem.
The most impactful documentation item that effects CMI is diagnosis. A physician can provide the exact same level of care for the same patient but the reimbursement numbers can vary widely based on what the physician documents. Optimally documenting CMI requires an accurate primary diagnosis because that diagnosis determines the Medicare Severity Diagnosis Related Groups (MS-DRG).
It is important to impart on your providers that the MS-DRG assigned is impactful and that adding additional diagnosis increases complexity and relative weight assigned by Medicare. This requires a working knowledge of the major complications and co-morbid conditions commonly associated with each DRG and documenting them appropriately. For example, appendicitis should be documented as acute appendicitis when appropriate and paired with any relevant secondary diagnosis such as generalized or localized peritonitis or perforation. The more accurate detail reflecting actual care complexity, the better the CMI and the more revenue realized through insurance reimbursement and collections.
Consistent Review and Continuing Education
In addition to initial onboarding training, we attribute much of our documentation optimization success to our ongoing documentation review efforts. After a couple of months of working, our providers have a personalized 1:1 live/virtual training session with Dr. Halem during which they review recent documentation to address areas of potential improvement. On an ongoing basis, we host group documentation lectures live on Zoom at a few different times a month (to accommodate varying schedules) so providers have the opportunity to ask questions and discuss real-world situations related to documentation.
The Results
Increased CMI results in higher reimbursement and lower adjusted cost per patient per day, which equates to a significant revenue enhancement for hospitals. Not only that, it also positively impacts Observed Over Expected (O/E) ratios for quality scores, including mortality and expected complications. As CMI increases, so do quality and HAC scores, which impacts quality ratings such as Leapfrog, Healthgrades, and Medicare Star ratings.
Since improved CMI has such a meaningful impact on revenue and care quality, we make CMI documentation training a priority. Through our focused onboarding and continued documentation education program, we consistently see significant rises in CMI. Below are a few recent examples of success we have seen with this approach:
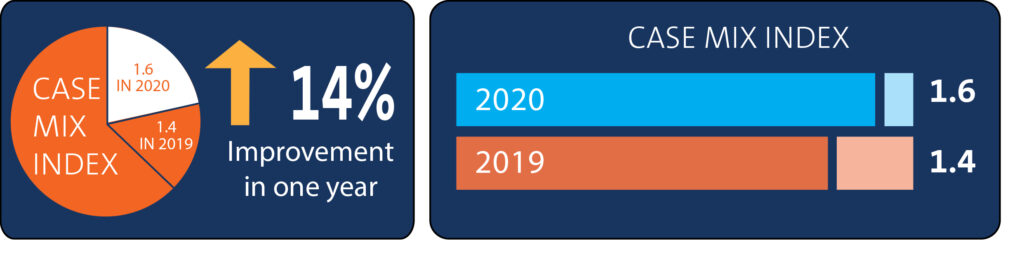
At one hospital these efforts resulted in a 14.3% increase in CMI within one year.
At another hospital, we saw a 23% increase in CMI the first year and an additional 28.4% increase after a second year of focused documentation improvement.
If you are interested in increasing CMI at your hospital, contact us to learn more.